THE ROBOTS ARE COMING
But should we be worried they are going to take our jobs?
Posted by Mike FitzGibbon on November 18, 2018
The robots are coming and, if the
headlines are to be believed, jobs as we know them are doomed.
But forgive me if I’m not running for
the hills – or reconsidering my choice of industry – just yet.
In fact, quite the opposite.
Unless you live in a news-free bubble,
you’d be aware advances in machine learning and Artificial Intelligence (AI)
are likely to drastically change the jobs of the future. Some claim
between 30 and 80 per cent of the jobs we do today will become obsolete.
The insurance sector is seen as
fertile ground for this ‘invasion’ - given its relative lack of disruption and
innovation to date - with the claims space in particular
considered ripe for the taking.
The Guardian was one of a host of
international outlets that picked up and ran with this story from Japan recently:
“A future in which human workers are
replaced by machines is about to become a reality at an insurance firm
in Japan, where more than 30 employees are being laid off and replaced
with an artificial intelligence system that can calculate payouts to
policyholders.”
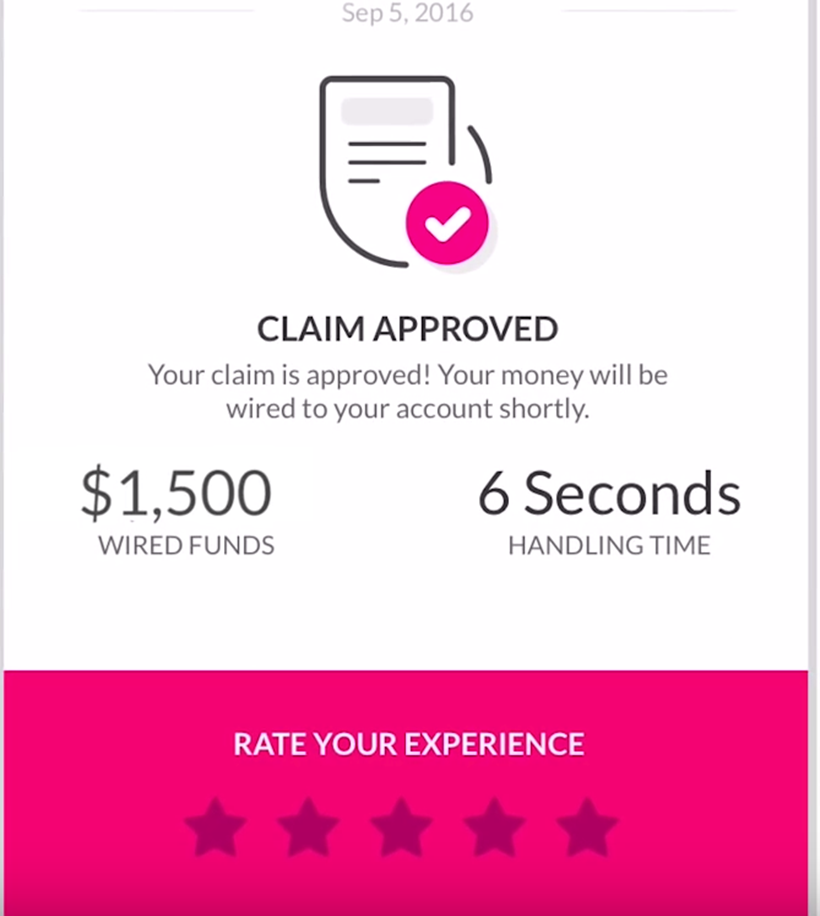
Insurance newcomers like ‘Lemonade’,
meanwhile, are adding to the hype with promises of using technology to pay
claims within 6 seconds.

Yes, significant changes as a result
of technology are inevitable. But does this mean the roles we know today will
disappear completely?
No. And conversely, the opportunity for
new and improved roles in the coming years looks more promising than ever.
Here are four reasons I don’t see robots
taking the job of claims managers in the area I work in; life insurance.
1. Technological
change happens slower than we think
Consider the fact that as much as 80
per cent of all life insurance claims are still submitted as a hard copy form.
Forget about a robot doing anything,
we haven’t even digitised the form!
This is despite the technology to
submit forms electronically having been widely available for more than 20 years.
Most would agree an online form is
the superior channel for the customer, the insurer and the environment, yet it
is still not common practice.
Why? Well technology is not the
constraint; it’s the ability and willingness to change the existing process.
The considerable cost and effort
needed for change requires evidence of a significant return on investment - and
it’s not really there.
The life claims sector has an even
bigger challenge: Even if we can get a claimant’s information online or over
the phone, will we get doctors and other third parties to use an e-channel to
submit documents?
This will remain one of the biggest
challenges in the industry, despite the technology required being basic and
available.
2. It’s about
gathering more than deciding
A supposed benefit the robots will be
able to bring is making an accurate decision instantly.
Lemonade’s six-second claims
decision is sold as a game-changing experience.
But there is a significant flaw.
Making a quick decision is
easy. We can say ‘yes’ to any claim the instant it is submitted if we
decide to but, of course, we don’t.
We accept that to make an accurate
decision there needs to be some due diligence.
As an example, 95 per cent of group
Total and Permanent Disability (TPD) claims are accepted. It’s simple to
demonstrate that paying 100 per cent of claims - and dismissing the claims team’s - is not cost
effective, and not good business.
Putting cost and effort into ensuring
only valid claims are paid is a value-add exercise. The challenge,
therefore, has always been to gather the necessary facts to make the right decisions.
So robots must tackle the real issue - getting
information from medical parties, employers and other stakeholders.
This is a much bigger challenge than
simply making a decision at speed.
3. It’s
not worth the risk
There is already work going on to
build models that can accurately determine the likelihood of a claim being
declined, based on available claims data.
If that 5 per cent discrepancy mentioned
above for TPD claims can be detected by the robots , there
is obviously a benefit to be had.
I’ve tried myself to build machine
learning models using 10 years of claims history to see how well those 5 per
cent of invalid claims could be identified.
I’ve failed, dismally. I never really
had a chance.
How good does my model need to be
before I can say the productivity benefit it will provide (by replacing the
case manager with the robot) outweighs the risk of making an incorrect
decision?
The answer is: between 99-100%
accurate.
Why? Because any incorrect decisions
that could cost on average $250k will quickly dwarf the resource cost savings.
Further studies of declined claims
show root causes are often so complex that a machine model would struggle to
get anywhere near 80 per cent accurate, let alone 99..
In summary, there is just not enough productivity
benefit to be had to justify taking the chance.
4. The 80-20 rule means it doesn’t
make sense
Of course, robots don’t have to do
all the claims. You could have a hybrid.
Perhaps the robots can process the
simpler claims and leave the costly humans to focus on only those claims where
their advantage makes sense.
This is already happening.
Triaging low-risk claims is something our robots can assist with.
But how much benefit will this
deliver? That is, how many case managers will it eliminate? Probably not
many.
The 80-20 rule fits pretty well in the life insurance claims space. 80 per
cent of claims received are, in fact, pretty straight
forward - low-hanging fruit that could possibly be automated, albeit with some
risk.
Unfortunately for the robots, these
cases are also pretty simple for the humans, and that
80 per cent of claims volume only accounts for 20 per cent of the resource effort.
So even if every one of these cases
was automated, only 20 per cent of resources could be saved. And the likelihood
of automating that 80 per cent is low.
The risk of incorrect decisions of an
‘auto-accept’ process is such that most businesses would only be comfortable
with as much as 30-40 per cent being robot approved.
Optimistically, this would eliminate
5-10 per cent of the claims manager resource
costs. Not a great return for a significant investment and increase in
risk.
For that reason, it’s not something
that we would expect to see jobs being lost to in the near
future.
So am I cynical enough to believe that
the machine learning and AI will not have any impact on life insurance claims
processing? Absolutely not. There are huge benefits to be had.
My point is replacing the case
manager should not be the goal. It’s simply not worth it.
Improving the performance of the case
manager, however, is where the future lies.
Take a group of 10 case managers
doing the same job and measure their output and there will be plenty of
variation.
Not all claim managers are created
equal, it seems.
The potential benefits of having
those least-effective managers improve – to the level of the best - are
substantial.
Artificial Intelligence – the robots
- might just be the best tool to close that gap. By identifying what it
is that makes some managers better than others.
So I suspect the robots are coming, but
we have little to fear and plenty to gain.
ENDS